AI-Driven Simulated Patient Interactions for Medical & Healthcare Training
1. Executive Summary
Large Language Models (LLMs) such as ChatGPT are shifting from optional study companions to core infrastructure inside medical education. Eight recent peer-reviewed studies and educator-facing analyses converge on one conclusion: virtual standardized patients powered by ChatGPT significantly accelerate communication, history-taking, decision-making, and empathy training, while reducing reliance on expensive physical simulations.
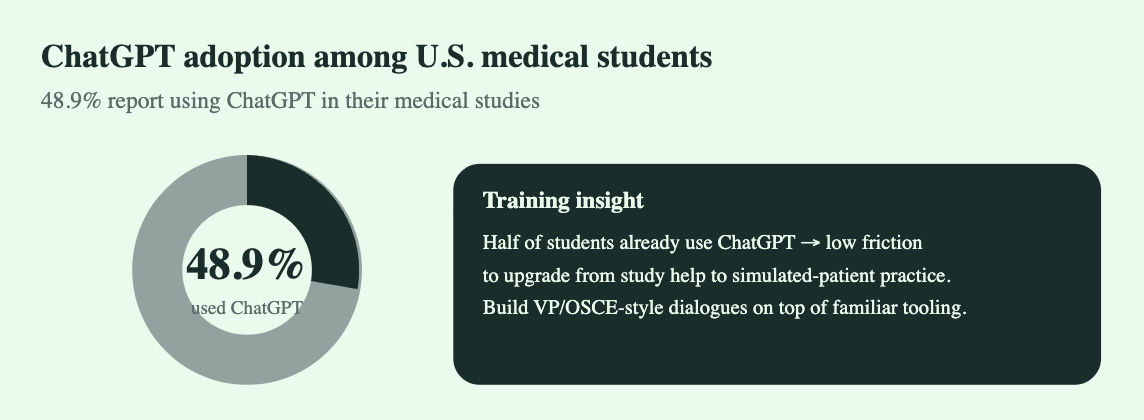
48.9% of U.S. medical students surveyed said they have used ChatGPT in their medical studies
In a survey of 415 students across 28 North American med schools, 52% reported using ChatGPT for medical school coursework
n a survey of 415 students across 28 North American med schools, 52% reported using ChatGPT for medical school coursework.
This whitepaper distills what the research actually proves, what it doesn’t, where AI-driven simulated patients perform well, where they fail, and how institutions can implement them safely.
2. Background: Why Healthcare Training Is Shifting to LLMs
Traditional simulation training depends on:
Human standardized patients (expensive, inconsistent)
Faculty time (limited)
Physical simulation centers (high CapEx)
Modern constraints — rising class sizes, shrinking budgets, increasing competency expectations — make scaling traditional patient simulations unsustainable.
LLMs, when configured correctly, can:
Role-play realistic patient personas
Provide branching interviews
Respond empathetically in text or voice
Offer immediate feedback on technique
Adapt difficulty to student level
Simulate rare or complex conditions on demand
This creates infinite, low-cost, high-fidelity practice loops.
3. Literature Review & Evidence Synthesis
3.1 AI as a Virtual Standardized Patient (VSP)
Source: “Clinical Simulation with ChatGPT: A Revolution in Medical Education?”
A GPT-4-based system simulated an acute coronary syndrome case.
Key finding: Medical students rated the interaction highly realistic, particularly the model’s emotional responses and adaptive questioning.
Implication: ChatGPT can replicate many of the teaching benefits traditionally requiring human actors.
3.2 Virtual Bedside Teaching Across Regions
Source: “Using ChatGPT for Medical Education: The Technical Perspective” (HKU/NUS)
Explored ChatGPT as the backend for virtual bedside encounters.
Key finding: Students reported improved confidence in history-taking and clinical reasoning.
Implication: LLM-based patients work across culturally diverse contexts and make bedside teaching more accessible.
3.3 Global Adoption & Attitudes
Source: “Current Status of ChatGPT Use in Medical Education”
Comprehensive review of 2023–2025 research.
Key finding: Students overwhelmingly view ChatGPT as beneficial for learning, with simulation activities ranked among top use cases.
Implication: Institutional adoption is accelerating due to bottom-up student pressure + top-down cost efficiency.
3.4 LLM Standardized Patients for Intern Physicians
Source: “AI-powered Standardised Patients: ChatGPT-4o’s Impact on Interns”
Evaluated performance on clinical case management tasks.
Key finding: Interns using the AI VSP demonstrated improved diagnostic reasoning and structured clinical thinking.
Implication: VSPs aren’t just for early training — they boost higher-level clinical judgment as well.
3.5 Mixed Reality + ChatGPT Virtual Patients
Source: JMIR Research “Integrating GPT-Based AI into Virtual Patients (MFR Training)”
Used GPT as the conversational engine inside a mixed-reality trauma scenario.
Key finding: Realistic patient communication significantly increased scenario immersion.
Implication: LLMs are becoming foundational for next-gen XR clinical simulations.
3.6 Empathy & Communication Training
Source: Springer “ChatGPT as a Virtual Patient: Empathic Expressions During History Taking”
Based on 659 interactions.
Key finding: ChatGPT demonstrated high consistency in empathetic, patient-centered dialogue. Students found it useful for practicing rapport and autonomy-supportive communication.
Implication: LLMs can equalize empathy-training quality without requiring trained actors.
3.7 Risks & Limitations Review
Source: “ChatGPT in Healthcare Education: A Double-Edged Sword”
Key finding: Major challenges include hallucinations, over-trust, lack of source transparency, variable clinical accuracy, and ethical concerns.
Implication: Without strong guardrails, VSP deployments can mislead or mis-train students.
3.8 Educator Adoption Perspective
Source: Lecturio “Using ChatGPT for Virtual Patients & Cases”
Key finding: Educators adopt LLM virtual patients primarily for convenience and consistency, particularly for case creation and OSCE prep.
Implication: Faculty see LLMs as extensions of traditional case-writing, not replacements.
4. Key Benefits Identified Across All Studies
4.1 Skill Acceleration
Faster improvement in history-taking
Better structure in clinical interviews
Higher confidence in differential diagnosis
4.2 Repeatability & Accessibility
Infinite practice cycles
On-demand cases (common or rare)
Suitable for early and late-stage learners
4.3 Emotional Realism
Studies consistently report:
Natural empathetic expressions
Realistic patient personas
Adaptable tone based on context
4.4 Cost Efficiency
Traditional simulation centers cost millions annually.
LLM-driven simulation reduces:
Faculty load
Standardized patient expenses
Infrastructure requirements
4.5 Scalability
Supports:
Massive cohorts
Remote learning
Cross-university collaboration
5. Risks & Ethical Considerations
5.1 Clinical Accuracy & Hallucinations
LLMs can produce incorrect medical facts.
Mitigation: Clinical guardrails, curated prompts, retrieval systems.
5.2 Over-Reliance
Students may mistake LLM replies as gold standard medical behavior.
Mitigation: Faculty-reviewed rubrics and structured debriefs.
5.3 Bias & Cultural Blind Spots
LLMs inherit training data biases.
Mitigation: Diverse prompting, demographic parameter controls.
5.4 Data Privacy
Any student-entered patient data must be synthetic or anonymized.
Mitigation: Strict privacy guidelines inside educational deployments.
6. Implementation Framework for Institutions
6.1 Phase 1 — Foundation
Select primary use case: history-taking, empathy, diagnostic reasoning
Set clinical accuracy constraints
Use GPT-4.1 or GPT-4o models with medical instruction tuning
6.2 Phase 2 — Virtual Patient Engine
Core capabilities:
Realistic persona behaviors
Emotionally adaptive responses
Multi-turn branching interview logic
Difficulty scaling
OSCE-mapped competencies
Safety + hallucination mitigation layer
6.3 Phase 3 — Integration
LMS integration (Moodle, Canvas)
Simulation lab workflows
Scoring & feedback dashboards
Faculty oversight modules
6.4 Phase 4 — Assessment
Use standard frameworks:
Calgary–Cambridge model
AAMC EPAs
OSCE checklists
Communication scoring rubrics
7. Global Adoption Outlook (2025–2028)
Near-Term (12 months)
All major medical schools will adopt some form of LLM simulation
Hybrid OSCEs combining human SP + AI SP become standard
XR + LLM training modules rise
Mid-Term (24–48 months)
AI Standardized Patients become a required curricular component
National exams integrate LLM-based practice modules
Research shifts from feasibility → optimization → accreditation readiness
8. Conclusion
The evidence is overwhelming: LLM-powered virtual patients are becoming one of the most impactful innovations in medical education since simulation centers were introduced. The technology is not a replacement for clinical training — it is an amplifier that allows every student to practice more, practice earlier, and practice safer.
The institutions that adopt this now will gain:
Better skilled graduates
Reduced training costs
Scalable simulation infrastructure
A competitive edge in medical education quality
This is a structural shift, not a temporary trend.