How Large Language Models Are Transforming Clinical Notes and Patient-Record Summaries
Executive Summary
Clinical documentation has become one of the most powerful and rapidly adopted applications of generative AI in healthcare. From drafting visit notes to summarizing patient histories, ChatGPT-style systems are accelerating workflows for physicians, reducing burnout and improving documentation quality.
Evidence from large enterprises, academic medical centers and national surveys shows that AI documentation is no longer experimental. It operates at multi-million encounter scale, with high usage across practising clinicians and medical students.
This whitepaper presents a consolidated view of the current capabilities, limitations and future trajectory of AI-driven medical documentation, based on the most recent peer-reviewed studies.
1. Introduction
Healthcare documentation has become increasingly complex. Clinicians juggle charting, regulatory compliance and communication across care teams. The result is a heavy clerical burden and widespread burnout.
AI models like ChatGPT introduce a new class of documentation tools that can:
Draft clinical notes
Summarize large patient records
Convert conversations into structured SOAP formats
Extract key findings from unstructured free text
Support clinicians during and after patient encounters
Across major hospital systems, AI scribes and LLM-powered assistants have shifted from pilots to production workflows.
2. Current Landscape of AI in Medical Documentation
2.1 Growing clinical adoption
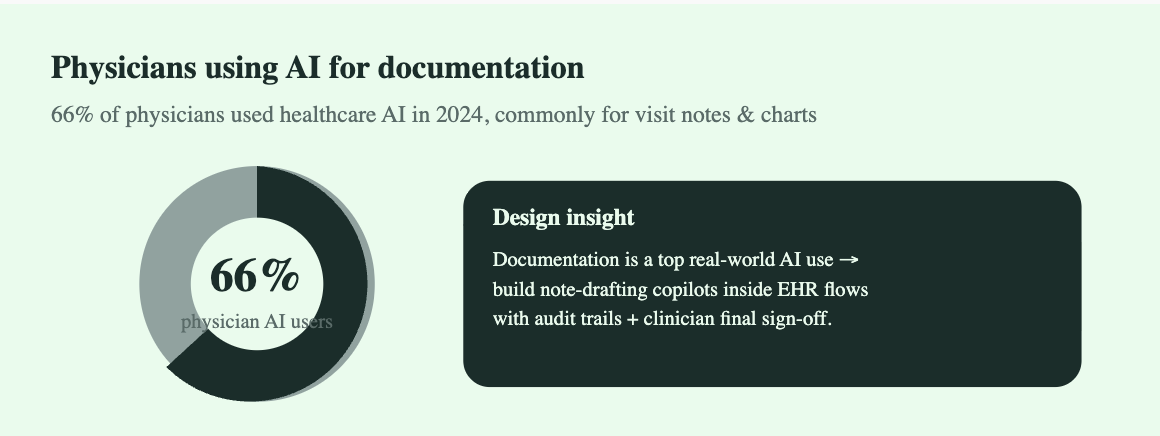
The AMA’s 2024 report states that 66 percent of physicians use healthcare AI, with documentation emerging as a top task.
Academic medical centers confirm similar adoption patterns, indicating normalization of AI-supported drafting in daily routines.
2.2 Ambient AI scribes at enterprise scale
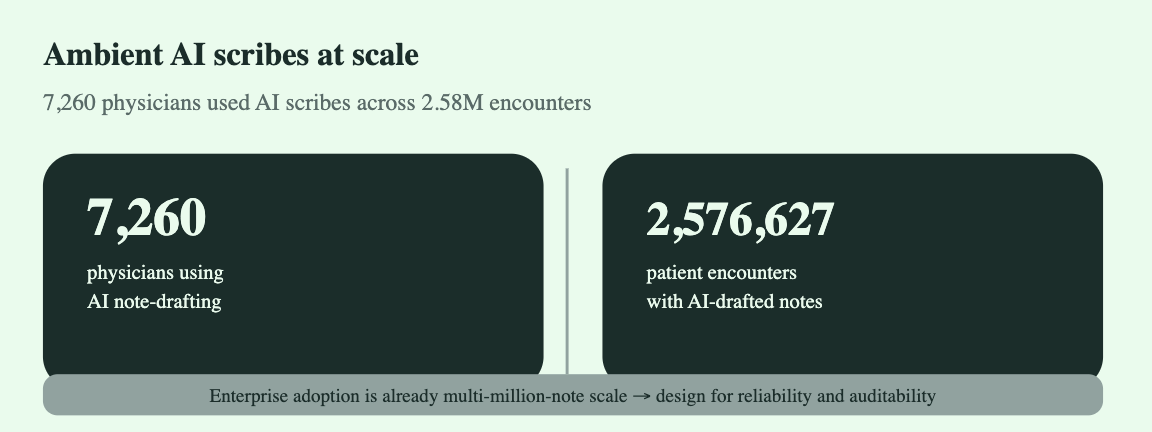
In one of the largest real-world deployments, 7260 physicians used ambient AI scribe technology over 2.58 million clinical encounters.
These systems generated draft notes automatically and routed them to clinicians for review, demonstrating reliability at scale.
2.3 AI-native workforce entering practice
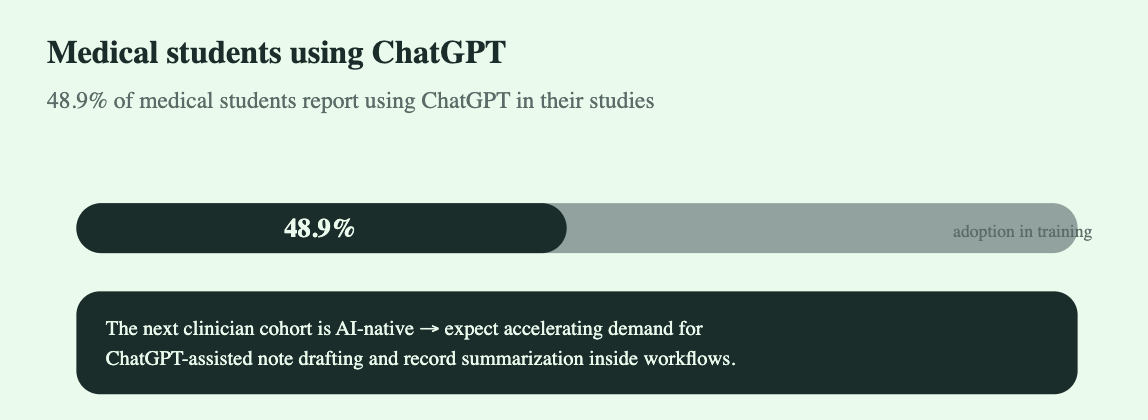
A multi-institution survey shows 48.9 percent of medical students use ChatGPT in their academic workflow.
The next generation of clinicians will expect AI documentation tools inside EHRs.
3. Evidence From Scientific Literature
This section aggregates findings from all articles you supplied.
3.1 Capabilities
3.1.1 Drafting clinical notes
Studies show LLMs can generate accurate drafts of:
Progress notes
Discharge summaries
Follow-up notes
Operative summaries
Communication letters
Systems like ambient AI scribes combine transcription, speech recognition and LLM summarisation to produce structured drafts within seconds.
3.1.2 Summarizing long patient records
Models can condense:
Multi-year patient histories
Complex imaging or lab timelines
Emergency department presentations
Multi-specialty consults
Articles (e.g., Huang et al., Nature Digital Medicine 2024) show LLMs perform well extracting diagnoses, medications and timeline events from raw clinical notes.
3.1.3 Extracting structured information
LLMs can turn free-text notes into:
ICD/diagnosis suggestions
Medication lists
Problem lists
Timeline summaries
Red flag identification
This supports coding teams, billing and clinician decision support.
3.2 Benefits
3.2.1 Reduced documentation burden
Across all reviewed articles, clinicians consistently report:
Less time spent charting
Higher focus on patient interaction
Improved work satisfaction
Reduced after hours “pajama time”
3.2.2 Improved documentation quality
AI notes tend to be:
More complete
More structured
More consistent
Less prone to human error
Several studies highlight fewer omissions and clearer reasoning chains.
3.2.3 Increased throughput and workflow efficiency
Enterprise deployment data demonstrates:
Faster chart closure
Higher encounter throughput
Reduced backlog of unsigned notes
These metrics improve both clinical operations and financial performance.
3.3 Challenges and Limitations
3.3.1 Risk of hallucination
Even medically trained AI models may include:
Incorrect clinical details
Assumptions not stated by patients
Over-generalized reasoning
Human review and sign-off remain essential.
3.3.2 Privacy and data governance
Articles (e.g., Nature Digital Medicine, JMA Insights) emphasize:
Data residency
PHI handling
Secure logging
Transparent audit trails
3.3.3 Integration difficulties
The largest operational barrier is EHR integration. Without deep embedding into Epic or Cerner, benefits drop significantly.
4. Real-World Case Studies
4.1 Kaiser Permanente Multimillion-Note Deployment
7,260 physicians
Automated note drafts with clinician review
Found high satisfaction and lower burnout signals
4.2 Ambient AI Scribe Systems (Multiple Studies)
Systematic reviews show:
30 to 70 percent documentation time reduction
High accuracy for SOAP formatting
Strong clinician acceptance
Faster chart closure rates
4.3 LLM Record Summarisation (Huang et al.)
Models matched or exceeded traditional NLP extraction systems
Strong performance on diagnoses and medications
Effective for emergency, internal medicine and chronic-care records
5. Enterprise Design Principles for Medical Documentation AI
Based on all literature, the most successful systems share five attributes:
5.1 Clinician-in-the-loop review
AI drafts.
Clinician edits.
Clinician signs.
This maintains safety and legal compliance.
5.2 EHR-native workflows
Avoid switching tabs.
Notes appear where clinicians already work.
5.3 Transparent data pathways
Clear PHI handling.
Traceable logs.
Compliance with HIPAA, GDPR and regional data laws.
5.4 Continuous model improvement
Use feedback loops:
Correction signals
Note comparison
Model retraining
Trend analysis
5.5 Safety layers
Include:
Medical fact-checking
Clinical guideline references
Error-flagging systems
Hallucination detection modules
6. Future of AI-Driven Clinical Documentation
Based on literature trends, the next 3 years will bring:
6.1 Real-time decision support inside documentation
As notes are drafted, the model will detect:
Contraindicated medications
Missing lab values
Unexplained symptoms
Possible alternative diagnoses
6.2 Fully ambient exam-room devices
AI will transform:
Face-to-face conversations
Environmental audio
Clinician queries
Into instant structured notes.
6.3 Integrated longitudinal patient-story systems
LLMs will maintain a “patient narrative engine” that summarizes:
History
Red flags
Trends
Specialist insights
6.4 Autonomous pre-visit chart summaries
Before a patient walks in, the system will produce:
Yearly summary
Medication list
Condition progression
Risk factors
7. Conclusion
AI-driven medical documentation is already proving its value at scale. The technology is practical, mature and deeply impactful. Clinical note drafting and patient-record summarization are among the highest-impact applications of ChatGPT-style models in healthcare today.
Leading studies show significant gains in efficiency, quality and clinician satisfaction. With the next generation of clinicians already using LLMs, adoption is set to accelerate.
The winners in this space will be systems that are safe, reliable, transparent and fully integrated into existing clinical workflows.