Multi-Agent Commerce in Healthcare
Orchestrating Insurance, Provider, and Pharmaceutical Value Chains Through Autonomous Coordination Systems
Abstract
Healthcare commerce represents one of the most structurally fragmented transaction ecosystems in modern economies, characterized by high regulatory oversight, multi-stakeholder incentive misalignment, and deep information asymmetry. Traditional digital health platforms have focused primarily on workflow digitization rather than systemic orchestration across insurers, providers, and pharmaceutical supply chains. This paper proposes a Multi-Agent Commerce Architecture (MACA) for healthcare that operationalizes care access and treatment fulfillment as an intelligent, distributed decision graph spanning clinical, financial, and logistical domains. We formalize the system around primary complexity drivers—clinical eligibility, network constraints, pre-authorization, and multi-entity orchestration—and propose a layered agent graph enabling adaptive, non-linear care pathways. The result is a paradigm shift from transaction digitization toward autonomous care commerce orchestration.
1. Introduction
Healthcare is not a single market but a federation of partially coupled markets, including:
Risk pooling and financial underwriting (insurance)
Clinical service delivery (providers)
Therapeutic manufacturing and distribution (pharma)
Unlike consumer commerce, healthcare transactions require simultaneous validation across clinical, financial, regulatory, and capacity domains before fulfillment can occur. A patient cannot simply “purchase” care; eligibility must be proven across multiple independent institutions.
Multi-agent systems provide a natural solution because they allow:
Local decision optimization at entity boundaries
Global objective coordination (outcomes + cost + access)
Continuous re-evaluation under uncertainty
The core thesis:
Healthcare commerce is best modeled as a constraint-satisfaction and optimization problem over a dynamic agent graph.
2. Primary Complexity Drivers
2.1 Clinical Eligibility
Clinical eligibility introduces probabilistic medical decisioning into commerce. Unlike retail eligibility (inventory or payment), clinical eligibility includes:
Contraindications
Evidence-based guidelines
Patient-specific biomarkers
Comorbidity interactions
This creates a biomedical constraint layer that is non-deterministic and continuously evolving with new evidence.
2.2 Provider Network Constraints
Insurance networks impose graph-theoretic limitations on provider accessibility:
Contractual pricing nodes
Geographic coverage clusters
Specialty scarcity pockets
Tiered reimbursement structures
This produces a topology optimization problem under cost and capacity constraints.
2.3 Insurance Pre-Authorization
Pre-authorization is effectively a risk-gated credit approval system for clinical procedures. It includes:
Cost prediction uncertainty
Fraud and utilization control
Evidence-based policy mapping
Temporal authorization windows
Pre-authorization loops create latency and abandonment risk, making them prime targets for agent automation.
2.4 Multi-Entity Orchestration
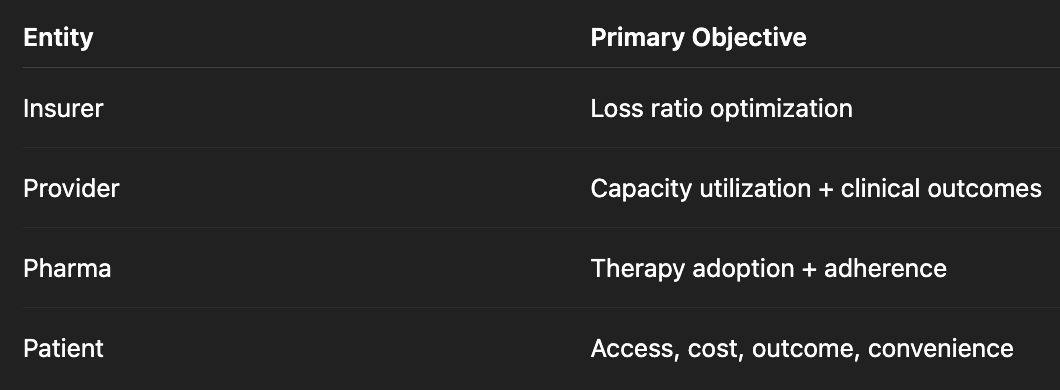
The most difficult challenge is coordination across entities with different objective functions:
Multi-agent orchestration allows Pareto frontier optimization across these competing goals.
3. Agent Graph Architecture
The proposed system operates as a stateful, event-driven agent graph.
Core Flow
Discovery
↓
Symptom / Need Triage
↓
Coverage Validation
↓
Clinical Eligibility Validation
↓
Provider Matching
↓
Booking / Transaction
↓
Care Navigation Support
This structure is not strictly sequential; it is a constraint resolution cascade.
4. Expanded Agent Layer Definitions
4.1 Health Intent Agent
Functional Scope
Transforms raw user signals into structured care intent.
Key Models
Symptom urgency classification
Preventive vs acute inference
Behavioral risk modeling
Technical Methods
Multimodal LLM triage models
Temporal symptom progression modeling
Risk scoring ensembles
4.2 Coverage Agent
Responsibilities
Real-time plan interpretation
Deductible state computation
Out-of-pocket projection
Complexity
Insurance benefits are effectively legal contracts expressed in semi-structured text, requiring hybrid symbolic + neural parsing.
Economic Impact
Reduces care abandonment due to financial uncertainty.
4.3 Clinical Eligibility Agent
Core Tasks
Treatment guideline mapping
Contraindication screening
Prior authorization prediction
Advanced Capability
Pre-emptive prior auth documentation generation.
This transforms prior authorization from a reactive step into predictive documentation assembly.
4.4 Provider Capacity Agent
Optimization Variables
Distance
Wait time
Specialty match
Outcome quality metrics
Mathematical Framing
Multi-objective optimization:
Minimize:
Travel_cost + Wait_time + Financial_cost
Maximize:
Outcome_probability + Patient_preference_score
4.5 Care Navigation Agent
Longitudinal Role
Extends beyond transaction into lifecycle revenue + outcome optimization.
Includes
Follow-up scheduling
Medication adherence prediction
Preventive intervention nudging
This agent converts episodic care into continuous care commerce engagement.
5. Non-Linear Pathways
5.1 Emergency Escalation Path
Discovery → Care Navigation → Provider Matching → Booking
This bypasses coverage certainty in favor of clinical risk minimization, reflecting real emergency care economics.
5.2 Insurance Block Loop
Coverage → Support → Coverage → Clinical Validation
This represents a feedback stabilization loop, where:
Documentation is generated
Coverage is re-evaluated
Clinical justification is strengthened
6. System Design Paradigms
6.1 Event-Driven Healthcare Commerce
Each agent publishes:
State changes
Confidence levels
Constraint violations
This enables asynchronous resolution across entities.
6.2 Federated Trust Architecture
Required because healthcare data cannot be centralized.
Likely stack:
Zero-knowledge eligibility proofs
Federated learning for triage
Privacy-preserving computation for coverage validation
7. Pharmaceutical Commerce Integration
Pharma enters at three points:
Clinical eligibility (therapy selection)
Financial assistance qualification
Adherence lifecycle monitoring
Future state:
Pharma agents dynamically offer outcomes-linked pricing contracts.
8. Economic Transformation Potential
For Insurers
Reduced unnecessary utilization
Faster pre-auth cycles
Improved loss predictability
For Providers
Higher schedule fill rates
Lower administrative overhead
Better patient routing
For Pharma
Higher therapy completion rates
Real-world evidence generation
Precision patient targeting
For Patients
Reduced cognitive load
Faster care access
Cost transparency
9. Failure Modes and Risks
Algorithmic Bias in Clinical Triage
Requires continuous audit and counterfactual simulation.
Network Gaming
Providers could optimize for agent ranking metrics.
Incentive Misalignment
Agents must operate under regulated objective functions, not pure profit optimization.
10. Future Research Directions
Autonomous Care Contracts
Smart contracts linking:
Clinical outcomes
Payment release
Manufacturer rebates
Self-Optimizing Care Pathways
Reinforcement learning across population outcomes.
Cross-Payer Shared Infrastructure
Industry-level agent interoperability standards.
Conclusion
Multi-Agent Commerce in healthcare represents a fundamental shift from fragmented workflow digitization toward autonomous care access orchestration. By decomposing healthcare transactions into distributed intelligent agents operating over a shared constraint graph, the industry can achieve simultaneous improvements in access, cost efficiency, and clinical outcomes. The long-term trajectory points toward a healthcare system where care pathways are dynamically assembled in real time, personalized across clinical, financial, and logistical dimensions, and continuously optimized through longitudinal outcome feedback loops.